Is HoFH hiding in your practice?

Homozygous familial hypercholesterolaemia
(HoFH) is an ultra-rare, inherited genetic disorder of lipid metabolism1,2
LDL-C=low-density lipoprotein cholesterol.
HoFH is characterized by:1-4
- Markedly elevated plasma levels of LDL-C (untreated LDL-C >10 mmol/L)3
- Premature atherosclerotic cardiovascular disease and cardiovascular morbidity and mortality
-
Cholesterol build-up:
- around the joints and on the tendons (xanthomas)
- in the eyes (corneal arcus) and around the eyelids (xanthelasmas)
The current estimated prevalence of HoFH is 1 in 300,000.4
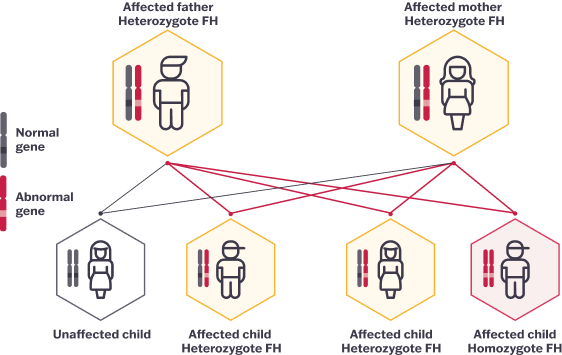
HoFH is an inherited lipid disorder
HoFH occurs when two pathogenic variants bearing the familial hypercholesterolaemia (FH)-
causing genes are inherited, one
from each parent.1
HoFH differs from HeFH
| Homozygous FH (HoFH)3 | Heterozygous FH (HeFH)3 |
|---|---|
| Pathogenic variants inherited from both parents | Pathogenic variant inherited from one parent |
| Occurs in 1 in 300,000 persons | Occurs in 1 in 250 persons |
| LDL-C >10 mmol/L (untreated) |
LDL-C ≥4.1 mmol/L in children LDL-C ≥4.9 mmol/L in adults |
| Likely physical symptoms, such as cholesterol deposits in the eye, tendons, knees, elbows and/ or between fingers and toes; these deposits are not always present | May have physical symptoms, such as cholesterol deposits in the eye, tendons, knees, elbows and/or between fingers and toes |
| Treatment at time of diagnosis, no matter the age, with a specialist | Treatment as early as age 8-10 |
Adapted from McGowan et al. 2019 and Cuchel et al. 2014
Look for HoFH in your practice
Physical signs and risk factors associated with HoFH:1,3,5
- Untreated LDL-C ≥10 mmol/L – lower levels should not be discounted if other factors are present
- Cutaneous or tuberous xanthomas – highly suggestive of HoFH in children
- Corneal arcus – highly suggestive of HoFH
- Evidence of CVD – in young children, early signs and symptoms are linked to aortic stenosis and regurgitation
- Family history of premature CVD
- Family history of HeFH
CVD=cardiovascular disease.
References
1. Cuchel M et al. Eur Heart J. 2023;44(25):2277-2291. 2. Raal FJ et al. Atherosclerosis. 2018;277:483-492. 3. McGowan MP et al. J Am Heart Assoc. 2019;8:e013225. 4. Tromp TR et al. Lancet. 2022;399:719-728. 5. France M et al. Atherosclerosis. 2016;255:128-139.